Jump-starting regeneration of injured nerves
Unlike in many other animals, injured nerve fibres in the mammalian central nervous system do not regenerate – at least not spontaneously. A lot of research has gone in to finding ways to coax them to do so, unfortunately with only modest success. The main problem is that there are many reasons why central nerve fibres don’t regenerate after an injury – tackling them singly is not sufficient. A new study takes a combined approach to hit two distinct molecular pathways in injured nerves and achieves substantial regrowth in an animal model.
Many lower vertebrates, like frogs and salamanders, for example, can regrow damaged nerves quite readily. And even in mammals, nerves in the periphery will regenerate and reconnect, given enough time. But nerve fibres in the brain and spinal cord do not regenerate after an injury. Researchers trying to solve this problem focused initially on figuring out what is different about the environment in the central versus the peripheral nervous system in mammals.
 It was discovered early on that the myelin – the fatty sheath of insulation surrounding nerve fibres – in the central nervous system is different from that in the periphery. In particular, it inhibits nerve growth. A number of groups have tried to figure out what components of central myelin are responsible for this activity. Myelin is composed of a large number of proteins, as well as lipid membranes. One of these, subsequently named Nogo, was discovered to block nerve growth. This discovery prompted understandable excitement, especially because an antibody that binds that protein was found to promote regrowth of injured spinal nerves in the rat. (It even prompted a film, Extreme Measures, with Gene Hackman and Hugh Grant – an under-rated thriller with some surprisingly accurate science and some very serious medical malfeasance).
It was discovered early on that the myelin – the fatty sheath of insulation surrounding nerve fibres – in the central nervous system is different from that in the periphery. In particular, it inhibits nerve growth. A number of groups have tried to figure out what components of central myelin are responsible for this activity. Myelin is composed of a large number of proteins, as well as lipid membranes. One of these, subsequently named Nogo, was discovered to block nerve growth. This discovery prompted understandable excitement, especially because an antibody that binds that protein was found to promote regrowth of injured spinal nerves in the rat. (It even prompted a film, Extreme Measures, with Gene Hackman and Hugh Grant – an under-rated thriller with some surprisingly accurate science and some very serious medical malfeasance).
Unfortunately, the regrowth in rats that is promoted by blocking the Nogo protein is very limited. Similarly, mice that are mutant for this protein or its receptor show very minor regeneration. What is observed in some cases is extra sprouting of uninjured axons downstream of the spinal injury site. This can lead to some minor recovery of function but it’s really remodelling, rather than regeneration.
But it does suggest an answer to the question: why would we have evolved a system that seems actively harmful, that prevents regeneration after an injury? Well, first, the selective pressure in mammals to be able to regenerate damaged nerves is probably not very great, simply because injured animals would not typically get the chance to regenerate in the wild. And second, it suggests that the function of proteins like Nogo may not be to prevent regeneration but to prevent sprouting of nerve fibres after they have already made their appropriate connections. A lot of effort goes in to wiring the nervous system, with exquisite specificity – once that wiring pattern is established, it probably pays to actively keep it that way.
There are a number of reasons why blocking the Nogo protein does not allow nerves to fully regenerate. First, it is not the only protein in myelin that blocks growth – there are many others. Second, the injury itself can give rise to scarring and inflammation that generates a secondary barrier. And third, neurons in the mature nervous system may simply not be inclined to grow. (Not only that – the distances they may have to travel in the fully grown adult may be orders of magnitude longer than those required to wire the nervous system up during development. There are nerves in an adult human that are almost a metre long but these connections were first formed in the embryo when the distance was measured in millimetres.)
This last problem has been addressed more recently, by researchers asking if there is something in the neurons themselves that changes over time – after all, neurons in the developing nervous system grow like crazy. That propensity for growth seems to be dampened down in the adult nervous system – again, once the nervous system is wired up, it is important to restrict further growth.
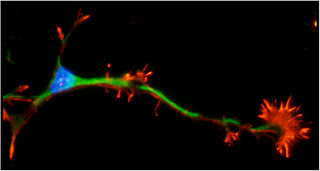
Researchers have therefore looked for biochemical differences between young (developing) neurons and mature neurons that have already formed connections. The hope is that if we understand the molecular pathways that differ we might be able to target them to “rejuvenate” damaged neurons, restoring their internal urge to grow. The lab of Zhigang He at Harvard Medical School has been one of the leaders in this area and has previously found that targeting either of two biochemical pathways allowed some modest regeneration of injured neurons. (They study the optic nerve as a more accessible model of central nerve regrowth than the spinal cord).
In a new study recently published in Nature, they show that simultaneously blocking both these proteins leads to remarkably impressive regrowth – far greater than simply an additive effect of blocking the two proteins alone.  The two proteins are called PTEN and SOCS3 – they are both intracellular regulators of cell growth, including the ability to respond to extracellular growth factors. The authors used a genetic approach to delete these genes two weeks prior to an injury and found that regrowth was hugely promoted. That is obviously not a very medically useful approach however – more important is to show that deleting them after the injury can permit regeneration and indeed, this is what they found. Presumably, neurons in this “grow, grow, grow!” state are either insensitive to the inhibitory factors in myelin or the instructions for growth can override these factors.
The two proteins are called PTEN and SOCS3 – they are both intracellular regulators of cell growth, including the ability to respond to extracellular growth factors. The authors used a genetic approach to delete these genes two weeks prior to an injury and found that regrowth was hugely promoted. That is obviously not a very medically useful approach however – more important is to show that deleting them after the injury can permit regeneration and indeed, this is what they found. Presumably, neurons in this “grow, grow, grow!” state are either insensitive to the inhibitory factors in myelin or the instructions for growth can override these factors.
They went on to characterise the changes that occur in the neurons when these genes are deleted and observed that many other proteins associated with active growth states are upregulated, including ones that get repressed in response to the injury itself. The hope now is that drugs may be developed to target the PTEN and SOCS3 pathways in human patients, especially those with devastating spinal cord injuries, to encourage damaged nerves to regrow. As with all such discoveries, translation to the clinic will be a difficult and lengthy process, likely to take years and there is no guarantee of success. But compared to previous benchmarks of regeneration in animal models, this study shows what looks like real progress.
Sun F, Park KK, Belin S, Wang D, Lu T, Chen G, Zhang K, Yeung C, Feng G, Yankner BA, & He Z (2011). Sustained axon regeneration induced by co-deletion of PTEN and SOCS3. Nature, 480 (7377), 372-5 PMID: 22056987


This comment has been removed by the author.
ReplyDeleteGood blog post. Interesting stuff...I have two questions, forgive me if I'm being an idiot...
ReplyDelete1) The PTEN/mTOR story is exciting - but surely there's a likelihood of tumour formation? Akt, downstream of PTEN is oncogenic. Indeed Akt-inhibitors are in stage 3 clinical trials for cancer.
2) Deletion of PTEN is an attempt to upregulate the capacity for protein synthesis in the CNS - a major intrinsic reason for its failure to regenerate. Reviews such as the following http://www.ncbi.nlm.nih.gov/pubmed/19520073 suggest the capacity in the CNS for *local* protein synthesis is very low, and that ribosomal protein P0 is undetectable past the axon initial segment. (This comes from Verma et al, 2005 though the actual experiment is an unpublished result).
Beyond the content and references of the review I linked above - does anyone know whether it has been proven that mRNA is locally transcribed, away from the cell body, in the adult CNS?
What am I missing in terms of the capacity of the CNS to locally synthesise proteins at synapses etc?
Hi Emily,
ReplyDeleteGood questions!
Regarding 1): This is of course a potential negative implication when trying to block any intrinsic signaling molecule, I think work would certainly need to be done to determine minimal effective dose as not to induce a tumerogenic state. Fortunately, it is possible that this drug could be injected directly into the CNS and depending on molecular size, may stay there (this would minimize systemic effects). Of course, depending on the kind of lesion that initiated the injury in the first place, the blood brain barrier may be compromised and allow drug to leak in... CNS injury is pretty messy!
2) Local protein synthesis can be quite high depending on the acidity state of the cell. Indeed, major aspects of plasticity are dependent on local protein synthesis and myelin-associated proteins such as MBP were some of the first proteins identified to have their mRNA transported great distances for local translation.
Colman, D. R., Kreibich, G., Frey, A. B. & Sabatini, D. D. Synthesis and incorporation of myelin polypeptides into CNS myelin. J. Cell Biol. 95, 598–608 (1982).
I think this is definitely so amazing on how this works here. Being able to regenerate the injured will be benefit so many. The research really paid off here.Movers Winnipeg
ReplyDeleteIt cannot be denied that a deep injury in spinal cord is going to be too risky for the victim of any violent attack, accident or medical negligence, and it might lead to paralysis or more devastating effects. It is the right of a sufferer and his family to file a spinal injury claim from anyone that are held responsible behind such a critical medical condition.
ReplyDeleteHire the locally based case management services for getting rid of all the medical and legal complications, after facing a heavy injury.
ReplyDeleteRegarding the speculations on "why would we have evolved a system that seems actively harmful, that prevents regeneration after an injury?". I was wondering if you could direct me to any papers exploring the explanations you suggest? I'm interested in reading further... Thanks, Tim
ReplyDeleteHuman brains are really amazing and mysterious.
ReplyDeleteOne must not forget to mention the consultation fee of the doctor, expenses on the tests and medicines, cost of medical equipment, fee of medical attendant, and the financial losses due to loss of earnings, while filing the papers for the spinal injury claim.
ReplyDeleteWould this treatment ,also ,work, for children suffering with cerebral palsy
ReplyDelete