Autism: The Truth is (not) Out There
Parents of a child affected by autism
naturally want to know the cause. Autism can dramatically disrupt the typical childhood
pattern of cognitive, behavioural and social development. At the most severe
end, the child may require care for the rest of their lives. Even at the milder
end, it may make mainstream education impossible and exclude many opportunities
available to typically developing children. Any parent would hope that knowing
the cause could lead to better treatment and management options for their
child.
 Parents should beware, however – while such
theories appeal to those common frustrations, they generally have no scientific
support whatsoever. Many of these are not just non-scientific, but actively anti-scientific
in nature. They tend to be based on anecdote, narrative and outright
speculation, rather than the scientific method (objective assessment of
empirical evidence). Many play to conspiracy theories, casting scientists and
doctors as pawns of Big Pharma, for example, and those proposing alternative
theories as brave mavericks fighting against the establishment to get The Truth
out there.
Parents should beware, however – while such
theories appeal to those common frustrations, they generally have no scientific
support whatsoever. Many of these are not just non-scientific, but actively anti-scientific
in nature. They tend to be based on anecdote, narrative and outright
speculation, rather than the scientific method (objective assessment of
empirical evidence). Many play to conspiracy theories, casting scientists and
doctors as pawns of Big Pharma, for example, and those proposing alternative
theories as brave mavericks fighting against the establishment to get The Truth
out there.
 The old psychoanalytical theory that autism
is caused by “cold parenting” has long since been discredited, but still pops
up every now and then (and is still quite prevalent in France and Argentina,
for some reason). It is often espoused by people who also happen to offer psychological
courses that purport to realign this relationship and thereby ameliorate the
condition. Bizarrely, this theory has been resurrected in modern form by neuroscientist
Susan Greenfield, who has suggested that autism is caused by overuse of digital
technology and immersion in social media, with a concomitant withdrawal from
direct human contact. The refrigerator mother has been replaced by the unfeeling
screen of the iPad.
The old psychoanalytical theory that autism
is caused by “cold parenting” has long since been discredited, but still pops
up every now and then (and is still quite prevalent in France and Argentina,
for some reason). It is often espoused by people who also happen to offer psychological
courses that purport to realign this relationship and thereby ameliorate the
condition. Bizarrely, this theory has been resurrected in modern form by neuroscientist
Susan Greenfield, who has suggested that autism is caused by overuse of digital
technology and immersion in social media, with a concomitant withdrawal from
direct human contact. The refrigerator mother has been replaced by the unfeeling
screen of the iPad.
 Another class of theories propose that
autism is caused not by an impoverished psychosocial environment, but by a
toxic physical environment. There is no shortage of potential culprits: fluoride
in the water, mercury in dental amalgam, vaccinations, genetically modified
food, herbicides, pesticides, food allergies, microwaves, cell phone towers, traffic
fumes, even toxins in everyday items like mattresses and dental floss.
Another class of theories propose that
autism is caused not by an impoverished psychosocial environment, but by a
toxic physical environment. There is no shortage of potential culprits: fluoride
in the water, mercury in dental amalgam, vaccinations, genetically modified
food, herbicides, pesticides, food allergies, microwaves, cell phone towers, traffic
fumes, even toxins in everyday items like mattresses and dental floss.
 In one sense, such arguments grant too much
credibility to these theories by allowing the battle to be fought solely on
their turf. It puts the onus on scientists to disprove each new theory. (This is like arguing with creationists
by trying to disprove the existence of Noah’s ark, instead of simply presenting
the positive evidence for evolution by natural selection). The problem with
this is that negative findings are simply not very compelling, psychologically,
regardless of the statistical strength of the conclusion. It’s too easy to
misinterpret what is really strong evidence that something is not the case as merely the absence of
evidence that it is (which would leave it an open question, requiring “more
research”). This means the “is not” side is at a disadvantage in an “is too”/“is
not” argument.
In one sense, such arguments grant too much
credibility to these theories by allowing the battle to be fought solely on
their turf. It puts the onus on scientists to disprove each new theory. (This is like arguing with creationists
by trying to disprove the existence of Noah’s ark, instead of simply presenting
the positive evidence for evolution by natural selection). The problem with
this is that negative findings are simply not very compelling, psychologically,
regardless of the statistical strength of the conclusion. It’s too easy to
misinterpret what is really strong evidence that something is not the case as merely the absence of
evidence that it is (which would leave it an open question, requiring “more
research”). This means the “is not” side is at a disadvantage in an “is too”/“is
not” argument.
 The results are dramatic – if one of
a pair of identical twins is autistic, the chance that the other one will be
too is over 80%, while the rate in fraternal twins is less than 20%. (Even in
cases when the co-twin does not have a diagnosis of autism, they very often
have some other psychiatric diagnosis, again much more so in identical than
fraternal co-twins). These results, which have been replicated many times, show
that variation across the population in risk of autism is overwhelmingly due to
genetic differences. Crucially, these results are not consistent with an
important role for variable environmental factors in the etiology of the
disorder – these should affect identical and fraternal twins equally.
Similarly, full siblings of someone with autism are at ~2 times greater risk
than half-siblings, again consistent with genetic but not with environmental
causation.
The results are dramatic – if one of
a pair of identical twins is autistic, the chance that the other one will be
too is over 80%, while the rate in fraternal twins is less than 20%. (Even in
cases when the co-twin does not have a diagnosis of autism, they very often
have some other psychiatric diagnosis, again much more so in identical than
fraternal co-twins). These results, which have been replicated many times, show
that variation across the population in risk of autism is overwhelmingly due to
genetic differences. Crucially, these results are not consistent with an
important role for variable environmental factors in the etiology of the
disorder – these should affect identical and fraternal twins equally.
Similarly, full siblings of someone with autism are at ~2 times greater risk
than half-siblings, again consistent with genetic but not with environmental
causation.
Unfortunately, until very recently, it has
not been possible to identify causes in individual children (with rare
exceptions). Science and medicine had apparently failed to solve this mystery. (I
say “had”, because, as we will see below, this is no longer true). The typical
experience of children and their parents in the health system has been one of
frustration, often with a long diagnostic odyssey, limited options for medical
intervention and a struggle to obtain access to specialised educational
services – all during a critical period in the child’s development. Given this
frustration, it is understandable that a variety of alternative theories of
autism causation have become popular.
 Parents should beware, however – while such
theories appeal to those common frustrations, they generally have no scientific
support whatsoever. Many of these are not just non-scientific, but actively anti-scientific
in nature. They tend to be based on anecdote, narrative and outright
speculation, rather than the scientific method (objective assessment of
empirical evidence). Many play to conspiracy theories, casting scientists and
doctors as pawns of Big Pharma, for example, and those proposing alternative
theories as brave mavericks fighting against the establishment to get The Truth
out there.
Parents should beware, however – while such
theories appeal to those common frustrations, they generally have no scientific
support whatsoever. Many of these are not just non-scientific, but actively anti-scientific
in nature. They tend to be based on anecdote, narrative and outright
speculation, rather than the scientific method (objective assessment of
empirical evidence). Many play to conspiracy theories, casting scientists and
doctors as pawns of Big Pharma, for example, and those proposing alternative
theories as brave mavericks fighting against the establishment to get The Truth
out there.
Ironically, the truth is that many of the people
pushing alternative theories are looking to make money off them – often by
taking advantage of vulnerable parents. Not all, by any means, but very often a
commercial interest is not hard to find (such as selling costly diets or
supplements or even more dangerous supposed “treatments”; claims that alternative therapies like homeopathy can
cure the condition; pricey seminars; or a new book to promote)*. Alternative theories
for autism and the treatments that go with them are big business.
The other irony is that these theories
actively ignore our growing knowledge of the real causes of autism, which are clearly
mainly genetic. The Truth is known but it’s not
out there. Scientists have done a poor job of communicating the extraordinary
advances made in the last few years in understanding the genetic causes of
autism. (Even many scientists and doctors seem unaware of these advances, in
fact). This leaves a void that can be filled by theories that are highly speculative
or sometimes frankly bizarre, and that are also either unsupported or flatly
contradicted by available evidence.
The
unusual suspects
 The old psychoanalytical theory that autism
is caused by “cold parenting” has long since been discredited, but still pops
up every now and then (and is still quite prevalent in France and Argentina,
for some reason). It is often espoused by people who also happen to offer psychological
courses that purport to realign this relationship and thereby ameliorate the
condition. Bizarrely, this theory has been resurrected in modern form by neuroscientist
Susan Greenfield, who has suggested that autism is caused by overuse of digital
technology and immersion in social media, with a concomitant withdrawal from
direct human contact. The refrigerator mother has been replaced by the unfeeling
screen of the iPad.
The old psychoanalytical theory that autism
is caused by “cold parenting” has long since been discredited, but still pops
up every now and then (and is still quite prevalent in France and Argentina,
for some reason). It is often espoused by people who also happen to offer psychological
courses that purport to realign this relationship and thereby ameliorate the
condition. Bizarrely, this theory has been resurrected in modern form by neuroscientist
Susan Greenfield, who has suggested that autism is caused by overuse of digital
technology and immersion in social media, with a concomitant withdrawal from
direct human contact. The refrigerator mother has been replaced by the unfeeling
screen of the iPad.
This technophobic notion is largely incoherent
and has no supporting evidence. (When asked for evidence, Greenfield has
described her own theory as follows: "I
point
to the increase in autism and I point to internet use.
That is all.”). The fact that autism is
typically diagnosed by two or three years of age, well before most kids have
Facebook or Twitter accounts, rather fatally undermines the idea.
 Another class of theories propose that
autism is caused not by an impoverished psychosocial environment, but by a
toxic physical environment. There is no shortage of potential culprits: fluoride
in the water, mercury in dental amalgam, vaccinations, genetically modified
food, herbicides, pesticides, food allergies, microwaves, cell phone towers, traffic
fumes, even toxins in everyday items like mattresses and dental floss.
Another class of theories propose that
autism is caused not by an impoverished psychosocial environment, but by a
toxic physical environment. There is no shortage of potential culprits: fluoride
in the water, mercury in dental amalgam, vaccinations, genetically modified
food, herbicides, pesticides, food allergies, microwaves, cell phone towers, traffic
fumes, even toxins in everyday items like mattresses and dental floss.
(These days, many of these are given a
pseudoscientific gloss by invoking the magic of “epigenetics”, a term now so
corrupted as to be worse than useless).
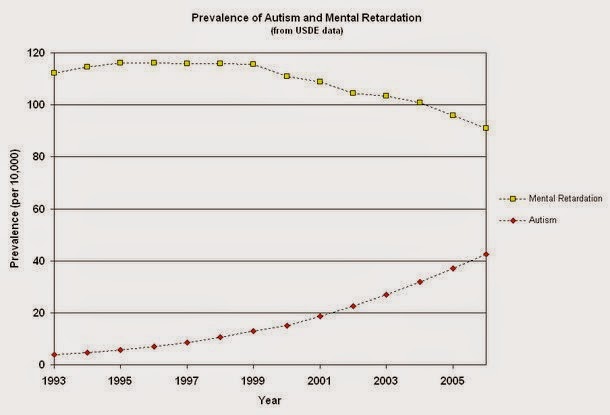
A driving factor behind all of these
theories is the fact that rates of autism diagnoses have been increasing
steadily in some countries for the past couple decades. This has led some to
declare “an autism epidemic”, with the obvious connotation that something in the environment must be causing
it.
This premise is flawed, however, as it
assumes the rate of diagnosis mirrors a real rise in the rate of the disease.
In fact, the rise in diagnosis rates can be largely explained by better
recognition of the condition among doctors and broader awareness among the
general public, and by diagnostic substitution, whereby children who previously
would have been given a general diagnosis of mental retardation are now more
commonly diagnosed with ASD. After all, prior to 1943, no one was diagnosed with autism
because the term had not yet been applied to this childhood condition. The
gradual rise in autism diagnoses following that period could hardly be thought
of as signaling a sudden epidemic. The criteria used by psychiatrists to define
the condition have changed multiple times over the years, including in the most
recent version of the DSM, and each change leads to a change in the number of children who fit under this diagnosis. The label is thus artificial and
changeable and its application has also varied widely over time. There is no reason
to think these variations reflect changes in the rate of the condition itself.
There is, moreover, no evidence linking any
of the potential environmental factors listed above to autism. In fact, in many
cases, there is very strong evidence disproving
any such link. (See here and here for a discussion of the absence of any link
with vaccination, for example). Regrettably, however, some of these stories
simply refuse to die.
Undead
memes
Part of their persistence may arise from
the way they are framed as anti-mainstream theories – for many adherents this
inoculates them against scientific critiques or counter-evidence, due to
mistrust of the scientific establishment or a lack of acceptance of the
scientific method as a means of objectively discovering the truth. It is, moreover,
very difficult to counter emotive personal anecdotes and highly publicised but
methodologically flawed studies (some of which have later been retracted or
even shown to be fraudulent), with, for example, dry statistical data showing
no epidemiological link to vaccines or fluoride or dental floss or any other
supposed environmental toxins.
 In one sense, such arguments grant too much
credibility to these theories by allowing the battle to be fought solely on
their turf. It puts the onus on scientists to disprove each new theory. (This is like arguing with creationists
by trying to disprove the existence of Noah’s ark, instead of simply presenting
the positive evidence for evolution by natural selection). The problem with
this is that negative findings are simply not very compelling, psychologically,
regardless of the statistical strength of the conclusion. It’s too easy to
misinterpret what is really strong evidence that something is not the case as merely the absence of
evidence that it is (which would leave it an open question, requiring “more
research”). This means the “is not” side is at a disadvantage in an “is too”/“is
not” argument.
In one sense, such arguments grant too much
credibility to these theories by allowing the battle to be fought solely on
their turf. It puts the onus on scientists to disprove each new theory. (This is like arguing with creationists
by trying to disprove the existence of Noah’s ark, instead of simply presenting
the positive evidence for evolution by natural selection). The problem with
this is that negative findings are simply not very compelling, psychologically,
regardless of the statistical strength of the conclusion. It’s too easy to
misinterpret what is really strong evidence that something is not the case as merely the absence of
evidence that it is (which would leave it an open question, requiring “more
research”). This means the “is not” side is at a disadvantage in an “is too”/“is
not” argument.
In my opinion, the strongest
counter-argument is one that is often not mentioned in such discussions – the
positive evidence for genetic causation. Instead of expending so much effort
trying to prove “it’s not that”, we can simply say “it’s this – look”. There is
really no explanatory void to fill. We know what causes autism, in general, and
we are identifying more and more of the specific factors that cause it in
individuals.
Autism
is genetic
The evidence that autism is largely genetic
is overwhelming – in fact, it is among the most heritable of common disorders. This
has been established through family and twin studies that look at the rate of
occurrence of the disorder (or statistical “risk”) in relatives of patients
with autism. If one child in a family has autism, the risk to subsequent
children has been estimated to be between ~10-20%, far higher than the 1% population
average. If two children are affected, the risk to another child can be as high
as 50%.
Now, you might argue that this does not
prove genetic influences, as environmental factors may also be shared between
family members. Twin studies have been designed for precisely that reason.
Here, we compare the risk to one co-twin when the other has a diagnosis of
autism, in two cases: when the twins are identical (or monozygotic, sharing
100% of their DNA) versus when they are fraternal (or dizygotic, sharing 50% of
their DNA). This design is so powerful because it separates genetic effects
from possible environmental ones. Genetic effects should make identical twins
more similar than fraternal twins, while environmental effects should not
differ between these pairs.
 The results are dramatic – if one of
a pair of identical twins is autistic, the chance that the other one will be
too is over 80%, while the rate in fraternal twins is less than 20%. (Even in
cases when the co-twin does not have a diagnosis of autism, they very often
have some other psychiatric diagnosis, again much more so in identical than
fraternal co-twins). These results, which have been replicated many times, show
that variation across the population in risk of autism is overwhelmingly due to
genetic differences. Crucially, these results are not consistent with an
important role for variable environmental factors in the etiology of the
disorder – these should affect identical and fraternal twins equally.
Similarly, full siblings of someone with autism are at ~2 times greater risk
than half-siblings, again consistent with genetic but not with environmental
causation.
The results are dramatic – if one of
a pair of identical twins is autistic, the chance that the other one will be
too is over 80%, while the rate in fraternal twins is less than 20%. (Even in
cases when the co-twin does not have a diagnosis of autism, they very often
have some other psychiatric diagnosis, again much more so in identical than
fraternal co-twins). These results, which have been replicated many times, show
that variation across the population in risk of autism is overwhelmingly due to
genetic differences. Crucially, these results are not consistent with an
important role for variable environmental factors in the etiology of the
disorder – these should affect identical and fraternal twins equally.
Similarly, full siblings of someone with autism are at ~2 times greater risk
than half-siblings, again consistent with genetic but not with environmental
causation.
These kinds of analyses answer the
question: in a given population at a given time, why do some people get autism
while others don’t? The answer is unequivocal – this is overwhelmingly
down to genetic differences.
Finding
mutations in specific genes
The fact that autism is largely a
genetic disorder has been known for decades. What has not been known is the
identity of the specific genes involved, with the exception of a couple
examples, involving genes associated with syndromes in which autistic symptoms
are common, such as Fragile X syndrome or Rett syndrome. These syndromes are
caused by mutations in specific single genes and account for 3-4% of all autism
cases. However, the vast majority of cases were left unexplained, and not for
want of looking.
This apparent failure to find the
specific genes involved clearly has led to the impression that genetics can not
explain the condition and that other factors must therefore be involved. This
is not the case at all – even if we remained completely ignorant of specific
causes, the fact that autism is extremely highly heritable would remain just as
true. As it happens, the failure to find specific causes had a technical reason
– it was simply very difficult to discover the kinds of mutations that cause
the condition. This is because such mutations are individually very rare in the
population and because there is not just one gene involved, or two, or even
ten, but probably many hundreds.
These mutations are now detectable
thanks to new technologies that allow the entire genome to be surveyed (either
for changes to single letters or bases of DNA or for deletions or duplications
of bits of chromosomes). Using these technologies, it has been possible to find
over a hundred different genes (or regions of chromosomes) in which a mutation
can lead to autism. Collectively, the known causes now account for 20-25% of
cases of autism.
It is worth emphasising that point:
doctors and clinical geneticists can now ascribe a specific genetic cause to perhaps
a quarter of individual autism patients. This is a vast increase from even a
few years ago and new risk loci are being discovered at an ever-increasing
rate. There is every reason to think we are only at the beginning of these
discoveries as we have really just begun to look. Again, regardless of how many
cases we have explained currently, the very high heritability of autism remains
a fact – the important factors in the vast majority of the remaining cases will
still be genetic. Far from being a failure, modern genetics has been
extraordinarily successful at uncovering specific causes of autism.
Autism
can be genetic, but not inherited
One common objection to the idea that
autism is a genetic condition is that so many cases of autism are sporadic –
they occur in a family where no one else has autism. How could it be the case
that the condition is genetic if it
is apparently not inherited? This
situation can arise when the condition is caused by a new mutation – a change
in the DNA that occurs in the generation of sperm or egg cells (mostly sperm,
as it happens). These occur all the time – this is how genetic variation enters
the population. Most of the time these “de novo” mutations have no effect, but sometimes they disrupt an important
gene and can result in disease. When they disrupt one of the many hundreds of
genes important for brain development, they can result in autism.
It has been estimated that as many as
half of all autism cases are caused by de novo mutations. By comparing the sequence of an affected child’s genome
with that of their parents it is possible to tell whether a mutation was
inherited or arose de novo. This is
obviously important information in assessing the risk in that family to future
offspring – in the case of a de novo
mutation, this should not be higher than the population baseline risk. By
contrast, if the mutation was inherited, then risk to subsequent children may approach
50%.
Another important finding is that the
effects of such mutations are more severe in males than in females. Not all
carriers of the known disease-linked mutations actually develop autism. Some
develop other disorders, while some are apparently healthy and unaffected (or
at least have no clinical diagnosis). This means people can be carriers of such
a mutation but not have autism themselves. This is especially true for females.
In cases where a pathogenic mutation in an autism patient was inherited from an
unaffected parent, that parent is twice as likely to be the mother as the
father. Also, the mutations observed in female patients who do have a diagnosis
of autism tend to be much more severe than those observed in male patients.
These data are consistent with a model where the male brain is more susceptible
to the effects of autism-causing mutations than the female brain. This can
explain why an apparently unaffected couple can have multiple children with
autism.
These genetic findings also highlight a
fundamental point: autism is not a single condition. The clinical heterogeneity
has always been acknowledged (leading to the use of the term autism spectrum
disorder), but it is now also clear that is also extremely heterogeneous from
an etiological point of view. Autism is really an umbrella term – it refers to
a set of symptoms that can arise as a consequence of probably hundreds of
distinct genetic conditions.
Defining
new genetic syndromes
Those distinct conditions were never
obvious before, because we had no way to distinguish between people who carry
mutations in different genes. But now genomic technologies can identify people
with the same mutations and are allowing clinicians to define new syndromes,
which may be characterised by a typical profile of symptoms. For example,
mutations in a gene called CHD8 are a
newly discovered, very rare cause of autism, but enough cases have now been
studied to define a symptom profile, showing for example that these patients
are at especially high risk of co-morbid gastrointestinal problems (found at
higher rate in autism generally, but not in all cases). Knowing the cause in
individuals can thus provide important information on prognosis, common
co-morbidities, even responsiveness to medications.
The application of genetic testing in
cases of autism should spare many children and parents the diagnostic odyssey
that many currently suffer through. A definitive diagnosis can bring important
benefits in terms of how families think of and deal with the condition. Indeed, support groups have arisen for many rare
genomic disorders, allowing parents to compare experiences with other families
with the same condition. On the other hand, as described in a recent review on
this topic: “we
should balance our enthusiasm
for finding a genetic diagnosis with
the recognition that autistic
traits represent one aspect of a
diverse behavioral spectrum, and
work to avoid any potential
stigmatization of the patient and
family through identification of
genetic susceptibility”.
The use of genetic information in
clinical management is likely to become increasingly important in the near
future as we learn more about newly discovered syndromes and their underlying
biology. This kind of personalised medicine is already happening in other fields,
such as oncology. One can hope that its application in psychiatry will go a
long way towards transforming the experiences in the health service of autism
patients and their parents and reducing the frustrations that arose when we
were effectively operating in the dark.
This is a positive message of real
success in science that is already changing how we think about disorders like
autism and that is likely to completely transform the practice of psychiatry,
especially for neurodevelopmental disorders. Scientists need to do a better job
of getting that truth out there.
*(For the record, I declare no such
conflicts myself).
Thanks to Dorothy Bishop, Svetlana Molchanova and Emily Willingham for helpful comments on this post.





The theory presented in this article relies upon the assumption that twin studies control for environment. However, several studies have shown this assumption does not hold. http://www.ncbi.nlm.nih.gov/pubmed/16238870
ReplyDeleteFurthermore, this article fails to acknowledge the work of several groups that have shown strong correlations between maternal infection, maternal autoimmune disease, maternal antibodies aimed at fetal brain proteins, proximity to high levels of pollution, etc. It is unwise to rule out an environmental component simply because of several "undead memes".
Twin studies do control for the environment, especially for things like maternal exposures. If these were causing autism, then dizygotic twins should both be affected at the same rate as monozygotic twins.
DeleteEpidemiological studies have found slightly increased risk of autism with maternal infection or obstetric complications - however, these statistical effects are minor when compared with the overall genetic effects. (In addition, obstetric complications may be an effect rather than a cause of a neurodevelopmental disorder).
Moreover, those factors are correlated with increase risk for other disorders too, such as schizophrenia and intellectual disability. If one is appealing to them to explain the apparent rise in autism (diagnoses), then one would have to explain why those other disorders are not also rising in prevalence.
What about countries like Italy where autism is still largely unheard of or seen. Italy is an interesting case as it's one of the very few modern countries that still eat fresh food as standard and have very close family bonds.
ReplyDeleteThanks for the excellent piece, Kevin. I'd like to draw you out a bit further regarding the role of environmental influences. After being a doubter, I've grown more agnostic regarding the possibly increasing prevalence of autism, but it's not my area. I wasn't aware of the trend toward decreasing MR dx's. That should certainly be part of the discussion. But leaving that debate aside, it still seems that environmental effects -- mainly intra-uterine -- get short shrift. The 77% unexplained etiology (and the similar number in schizophrenia, which I know more about) stands out. I'd probably argue, gloomily, that what we know about etiology for both categories is probably considerably less than those percentages suggest.
ReplyDeleteI agree that twin studies offer strong support for genetic etiology, but it seems that twin study commentary downplays some well-known differences and variations in the intra-uterine experience of mono- vs dizygotic twins. Most agree that autism and schizophrenia are neurodevelopmental disorders. And it is fairly clear that a developing human is never more environmentally sensitive and plastic than during the nine months after conception, which, presumably, makes us subject to subtle developmental 'butterfly effects.' John McGrath (among others) has written persuasively about a number of environmental gradients that may influence gestation in schizophrenia – e.g., rural to urban, summer to winter (or dark to light), immigrant status. How many variables might be in play? Nutrition, vitamins, hormones, activity levels, social stress, differences in allergens and pathogens, immune system activation – and all interacting dynamically with genetics. I don't know the autism literature about these sorts of gestational influences. But I feel about this area like I feel about complex genetic interactions -- even in the absence of good evidence and adequate analytical tools, it has to be critical.
Thanks Dwight, for your comments. Regarding possible intra-uterine effects, I agree they may be important and, in some cases, could even be causal (like with valproate, for example). But I also think they are not likely to be of major importance as causes or sources of variance across the population, due to the twin and family studies, which all show much higher concordance in MZ than DZ twins. I see little reason to think that an external environmental factor (external to the twins, that is) would have more shared effect on MZ than DZ twins. These studies also consistently show no effect of a shared family environment.
DeleteJohn McGrath has written a chapter on environmental factors (and gene by envt interactions) for an upcoming book that I am editor of on The Genetics of Neurodevelopmental Disorders. He covers many epidemiological findings of "risk factors" which include the ones you list above and others (obstetric complications, maternal infection). Most show very modest effects and the problem with epidemiological studies is that inferring causation and eliminating confounds are both effectively impossible.
I should also say that all the environmental risk factors that have been identified in epidemiological studies are also associated with statistically increased risk of schizophrenia and neurodevelopmental disorders more generally. Thus, if one is appealing to changes in those kinds of factors as an explanation for increasing rates of autism diagnoses, you'd have to additionally explain why rates of schizophrenia are not also increasing.
DeleteAlso Kevin Mitchell, you wrote, "you'd have to additionally explain why rates of schizophrenia are not also increasing". Since autism is associated with a higher risk of schizophrenia, and autism rates are increasing, if we waited twenty years for the boys, and thirty-five years for the girls, I think we would see an increase in schizophrenia rates.
Delete